Will proposed updates to the Hospital Price Transparency rules compel compliance from reluctant hospitals?
Federal regulations requiring hospitals to publish data on the prices of their services went into effect on January 1, 2021. The Hospital Price Transparency Rule expands upon requirements imposed through the Affordable Care Act, mandating that hospitals publish not only their chargemaster gross prices, but also discounted cash prices (the rates hospitals charge individuals who do not have insurance), payer-specific negotiated prices, and the de-identified range of prices that the hospital negotiated across all payers/third parties.
Price Transparency Rules 1.0: A Toothless Tiger?
Fast forward six months later, and reports begin to trickle in: the vast majority of hospitals are “unambiguously noncompliant” with the new regulations. A study sampling 500 hospital websites between May and July of 2021 found that only about 5% fully complied with the price transparency law; specifically:
- 80% failed to publish payer-specific negotiated charges
- 40% omitted discounted cash prices
- 52% did not publish any negotiated rates whatsoever
It gets worse. The Wall Street Journal found that hundreds of hospitals embedded code that actually obscures pricing data from popular search engines. Perhaps it’s no wonder then that only 9 percent of surveyed adults are even aware that these rules exist.
Some hospital executives allege that the cost of reporting pricing data – either stemming from the cost of aggregating data or from the potential fallout in negotiations with payers – is greater than the $300 per day fine hospitals face for non-compliance. Others claim to be waiting for additional clarification/guidance from CMS, or to gauge how their competitors respond to the regulations.
Sharpening the Tiger’s Teeth
In response, CMS announced on July 19 a new proposal to heighten the penalties hospitals face for noncompliance, and clarifies requirements around data accessibility. Specifically, the new rule would impose a sliding scale of penalties based on hospital bed count. Under the original rule, the maximum fine any hospital faced was $300 per day –$109,500 annually – which is pocket change for most large health systems. The new rule fines hospitals with over 550 beds $5,500 per day, resulting in forfeiture of over $2 million per year.
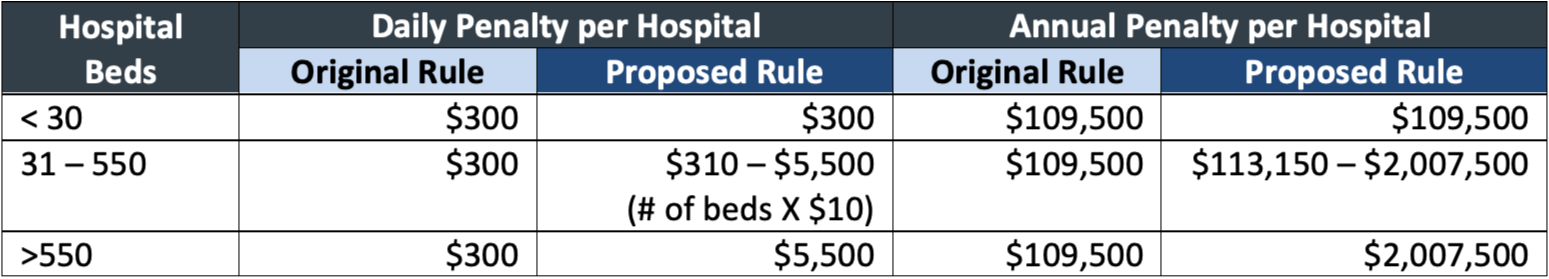
Source: https://public-inspection.federalregister.gov/2021-15496.pdf
CMS announced an intention to target hospitals that attempt to obscure their pricing data, mandating that standard charge information must be accessible through automated searches, and that machine-readable files must be posted through a link on a publicly available website.
Beyond these fixes, CMS strives to increase the utility and accessibility of pricing data through the following requirements:
- Hospitals’ price estimator tools must provide a single dollar amount based on the circumstances of the individual health care consumer
- Hospitals must provide use plain language in descriptions of the 300 required shoppable services
- Machine-readable files must be posted in a standardized format (CMS seeks input on what the standard should be)
All Bark and No Bite?
Will these updated penalties and clarifications compel hospitals into compliance? The jury is out, but the impact of the proposed updated rules depends heavily on enforcement. As it stands now, a noncompliant hospital first receives written notice that it is noncompliant, then receives a request for a Corrective Action Plan (CAP); if a hospital refuses to respond to or comply with the CAP, only then will CMS impose the daily fine. With so many interim steps before CMS brings down the hammer, a hospital that is reluctant to disclose its prices might not immediately change its mind.
For hospitals to change their behavior, the more convincing threat may not come from the government at all, but instead from public pressure and the media. As evidence, once the Wall Street Journal published its article exposing health systems who blocked their pricing data, many of the hospitals removed the code that obstructed search engine hits. In a separate but similar vein, a study out of Johns Hopkins University found that hospital lawsuits against patients declined 92% between 2018 and 2020; while some of the decline may be pandemic-driven, researchers believe that negative media attention significantly dampened hospitals’ appetites for pursuing unpaid bills through litigation.
It’s too soon to make predictions: the proposed rules – if they go into effect as written – won’t apply until January 2022. In the meantime, it’s incumbent upon health care purchasers, the media, and other stakeholders who care about hospital price transparency, to remain vigilant and hold hospitals accountable.
Photo by Max van den Oetelaar on Unsplash.

